My cancer is advancing again despite continuing treatment which is being stopped now. I am devastated. I am crushed. I am angry. The next pollyanna cheerleader who tells me "You got this!" is going to get punched in the face.
Be warned: this is not a happy post. Treatment options are running out and without finding something else that works I personally doubt I'll live to ring in 2022. This is not to say I am hopeless, only that I am living with my eyes open and have seen what happens to most cancer patients that fail multiple treatments. I just flunked folfiri.
In my previous blog post I wrote about the Covid vaccine and how it can cause artifacts on a CT scan that look like cancer, but aren’t. At the time, I had just had a scan that showed new artifacts primarily in my left lung, very close to the injection site, while everything below the diaphragm was greatly improved. Blaming the vaccine seemed suitable at the time, with the plan to do my next scan sooner than we normally would.
It’s now eight weeks later and I’ve been scanned and blood tested, and unfortunately the Covid vaccine is off the hook. This is genuine cancer in my lungs, and oh by the way my liver lesions are also growing again. Judging by my blood test numbers, the amount of cancer in me is approximately the same as it was in November 2020 when I ran as the only runner in my very own made-up Thanksgiving 5K. Except at the time there was no significant cancer in my lungs to slow me down.
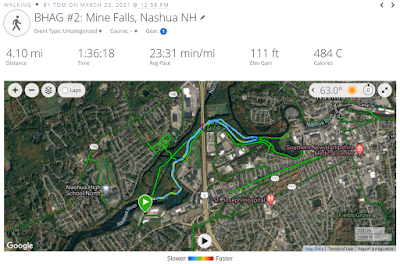
My fitness peaked in late March of this year, just before my Covid shot, and has been declining steadily ever since. In numeric terms I’ve gone from being able to cover multiple miles slightly slower than a 15 minute per mile pace to being only able to cover a single mile in a little over 20 minutes. It’s unclear how much this change is due to cancer in the lungs and how much is due to my anemic blood counts.
I hear whistling and wheezing sounds when I breath. It sometimes hurts to take a deep breath. It's like having a permanent low grade asthma attack which isn't relieved by my inhaler, though frequently Benadryl gives relief in exchange for drug induced fatigue. It really disturbs my attempts to meditate when focusing on my breath instantly reminds me of the deadly cancer in my lungs.
This overall is very bad news. My oncologist has not said I’m out of options, only that his well of ideas is running dry and I should talk to some “wicked smaht” people in Boston to see if they have any great ideas like a clinical trial or such. Thusly, next week I have an appointment with a specialist and researcher in my specific form of cancer to come up with a Plan A. We already have a Plan B, which I call “chemo leftovers”, and involves re-using chemo drugs that have worked on me in the past but in a new combination. One thing I dislike about plan B is that it involves irinotecan, the “iri” in folfiri, which I just flunked. I’d feel much better about plan B about a year from now, after the cancer has had a chance to become susceptible to all the ingredients again.
So how are we, that is my wife and I, doing? About as well as one would expect. Lots of crying, especially by me as I mourn the loss of the summer I dreamed of. This scan was supposed to show little to no cancer in the liver and lungs, I’d ask for my chemo to be dialed back, and have a very active summer of long walks, perhaps a bit of running, cutting firewood for the winter, further exploring our land in Vermont and cutting new trails. There were signs in my poor aerobic capacity that it might be a very bad scan, but I was hoping that was a side effect of chemo that would abate with less frequent treatments.
In a weird way, this bad scan is a relief. Think about it: for the past couple months my body has been telling me that things are getting worse, while family and friends encourage me to stay positive and hope for the best. Now I know why my body has been getting worse and there’s a chance something can be done about it and things might start improving. I’m cautiously optimistic, while also being fully aware that each successive cancer treatment is less likely to work and if it does work, is likely to fail sooner than the previous treatment.
But back to my wife and I. We’ve had some discussions that we never imagined having in our 50s. My wife has said that if it was her, she would have stopped treatment long before now, excepting maybe a clinical trial that would advance the science and help future patients. She has made it clear that I’m under no obligation to continue treatment just for the sake of her. As much as she’d like to keep me around as long as possible, she would like even more not to see me suffering.
For me personally, I’ve had enough experience with cancer treatments to know that many times they can get rid of the worst cancer symptoms, and the right treatment might just blow the cancer out of my lungs and allow me to go running again. But I’ve also experienced the absolute darkness that falls over my mind during part of every chemo cycle. I’ve felt the odd pains that can’t be explained other than saying “chemo” and taking an opioid to make it go away.
That said, I’ve lost my sense of urgency and am beginning to set limits on my doctors. At the beginning, cancer treatment is very standardized and the doctors stick to the standard protocols and don’t seek much input from their patients. As time has gone by, all the standard treatments have already been tried, we’re trying things outside the proverbial box, and my doctor actually asks “what would you like to do” after suggesting chemo leftovers. He also asked my wife what she thought.
My wife knows me very well, and suggested starting the chemo leftovers while at the same time setting up appointments with the experts in Boston. I liked the outline and added my own conditions: Yes, let’s plan to start the chemo, but I demand an extra week off to allow the healthy parts of my body to recover slightly. If the cancer continues to grow in that week so be it. I’ve been on constant chemo since last October and in that time have not so much as missed a week due to low blood counts.
Conveniently, that extra week allowed time to set up at least one appointment in Boston, which I can go to without a chemo hangover, and perhaps we’ll come up with a better idea than leftovers and can get started right away on that.
I also demanded that if we’re doing platinum chemotherapy again that the cycle length should be four weeks and there shouldn’t be any use of neulasta. Previously, three week cycles on platinum were exceedingly difficult and a number of cycles had to be lengthened to four weeks anyway. I also dislike neulasta because while it does a great job of raising my white blood cell counts, my other blood counts plummet. Neulasta is one of those drugs where everybody gets the same dose and for me it’s just too much of a good thing. Historically, my blood counts recover nicely on their own if given an adequate cycle time, like four weeks on platinum.
And as always, agreeing to chemotherapy, or any cancer treatment for that matter, doesn’t mean you can’t say “stop” at any point in the future. I am fully in the palliative phase of cancer treatment, where any treatment should be judged on whether it improves my quality of life or not. I will not suffer excessive side effects for the promise of better health in the future, because I’ve already been burned by that several times and the odds of getting a miracle response go down with each change in treatment.
In closing, let me say how aggressive neuroendocrine cancer is. I’ve heard that life expectancy is about a year, and judging from the other men I’ve known with the disease that seems about right as they’re all dead now and as far as I know I’m the last survivor of those diagnosed in early 2020. I know of only one guy who has made it to three years and he didn’t do it by chasing treatment after treatment. Instead, he had the exact same chemotherapy I had when first diagnosed, it stabilized his disease, and his disease remains stable to this day, three years later with no additional treatment. That is how most people survive cancer for years and years: They get years of success out of each treatment instead of just a few months, with time of stability for their bodies and minds to recover.
I unfortunately haven’t fallen into that pattern of prolonged success. I think it’s important that my family and friends realize that if I don’t find another treatment that works with tolerable side effects, this could turn out to be the beginning of the end. This isn’t a lack of hope, it’s a realistic assessment of my situation. An experimental drug could produce a miraculous response, but in the vast majority of cases it only provides a modest benefit, if any.
To end on a more positive note, here are some things you can do to help. For starters, please refrain from pollyanna cheerleading, as it only makes me reiterate the direness of my situation and that won't make either of us feel good. Also, no unsolicited medical advice please. Each cancer is unique and I'm already working with experts in the field, and I'm tired of explaining why certain treatments either don't apply to me or are snake oil.
With the don'ts out of the way, here are some do's: wish me well in my ongoing battle and allow me to whine a bit about the difficulties. Let's focus on the fight at hand and let the results be what they will. If you're religious (I am not), feel free to pray for me, but please don't proselytize. Most importantly, help me enjoy the day we have today and let's have a lot of laughs which really is the best medicine.
Despite my realistic and possibly depressing view of my situation, I really do have hope that some treatment will work spectacularly well for me and I'll live for years to come.